Choose your own path
Drug User Health Program
We provide new syringes, sterile water, mixers, and other safer injection equipment. You’ll also find safer smoking and safe snort kits, used syringe disposal, education, harm reduction information, and referrals for people who use drugs (PWUD) at no cost to you. The syringe program is anonymous, safe, and judgement free.
Emma’s Exchange is the syringe services program (SSP) administered by Open Aid Alliance and has been in operation since 2013. It is an anonymous, evidenced-based public health program that reduces infection and the spread of diseases such as HIV and hepatitis C among community members who inject drugs.
How to get supplies
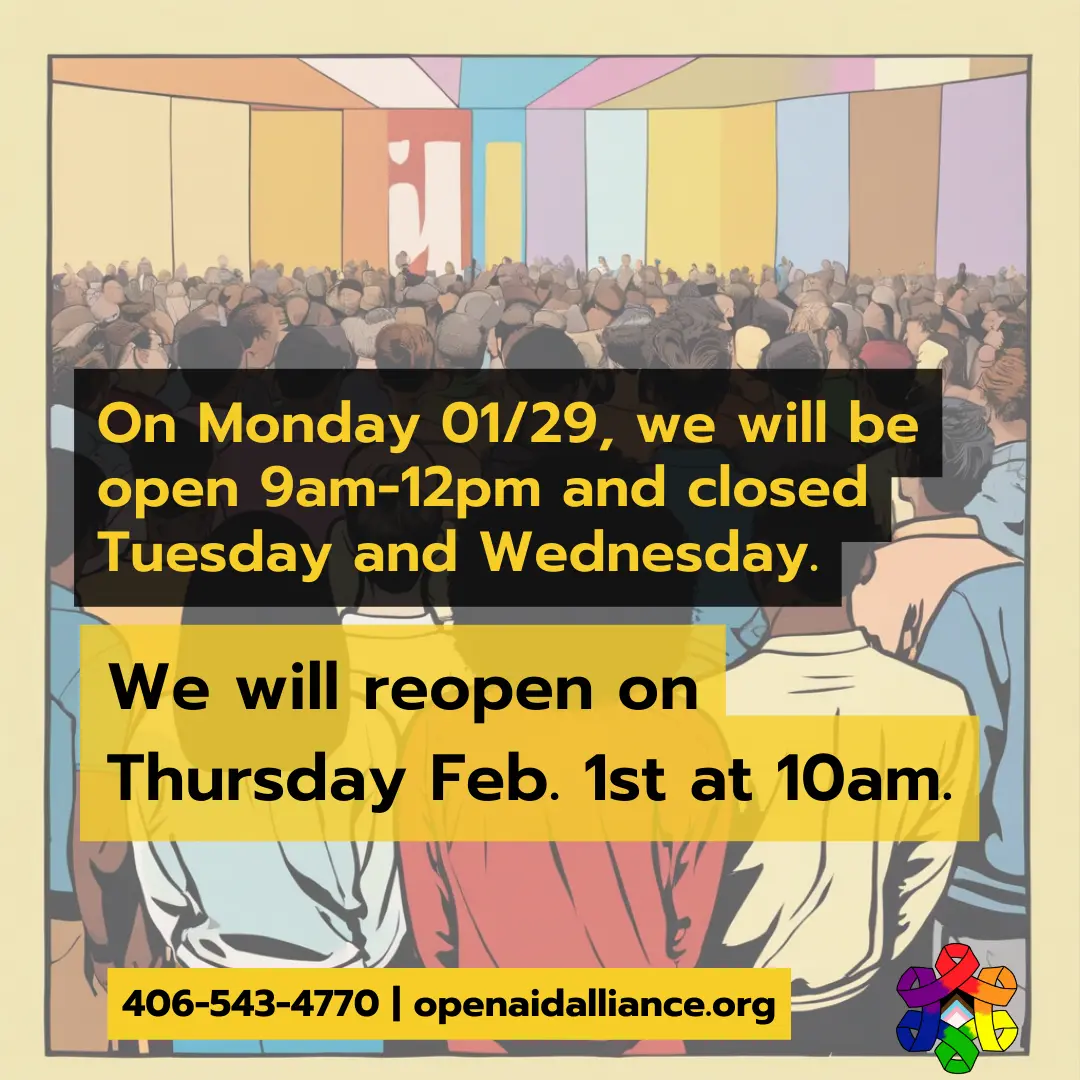
Missoula residents: Safer injection, smoking and snorting supplies can be picked up at 715 Ronan Street, Mondays-Thursday 10am-5pm. We are closed on Fridays. If you live outside Missoula, click the button below to order supplies sent directly to you at no cost.
We are able to ship within Montana only. If you are located in another state, please visit Nasen for possible services in your area.
Have questions?
If you have any questions on how the syringe services program operates or about the benefits of syringe services programs, check out our FAQ below.
August 31st
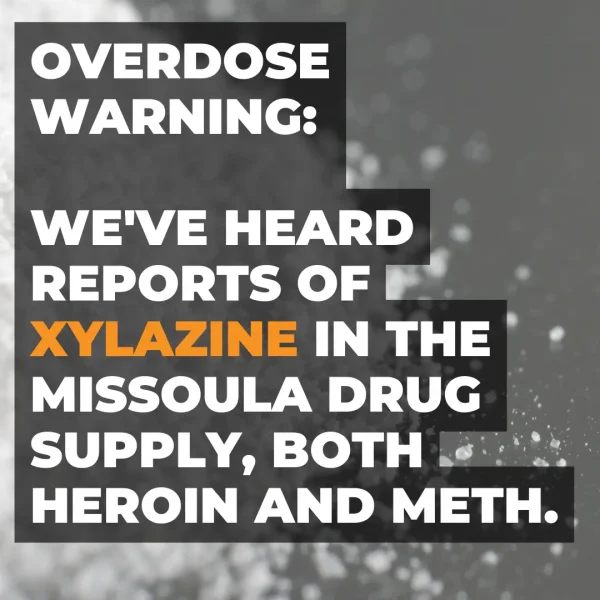



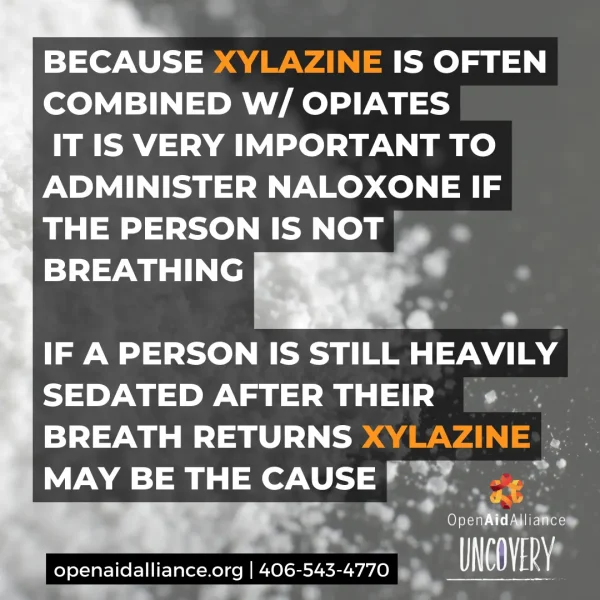
A warning about a dangerous cut found in the Missoula supply. Click the > to the right to read more. If you suspect Xylazine is in your dope, let us know next time you visit the SSP. We’ll help spread the word.
Follow Us On Social Media For All The Latest Information
We use social media to let people know about service changes, inventory updates, reports of bad drugs, new services, changes to our hours of operation, and more. If you want the latest on the SSP, follow us on Facebook, Twitter, and Instagram.
Here are additional resources to check out to stay safe and healthy
These are some of our favorite resources for folks who use injection drugs. Using best possible injecting practices, taking care of your injection sites and understanding overdose response are key to keeping yourself and those you care about healthy. And, as always, feel free to contact us with any concerns or questions at 406-543-4770.
Read and watch the story of how Emma’s Exchange came to be.
Check this out: Getting Off Right is an in depth guide of best practices for injection. One of our favorite publications. If you’re new to injecting, come in and ask for a copy or click the link to download a PDF copy.
Here’s a map of SSP’s around the country. Handy if you don’t live here or if you’re travelling.
Here’s a guide from the CDC about reducing your risks for HIV if you’re an injection drug user. HIV and Injecting Drugs 101
The CDC has a section of their site devoted to the effectiveness of SSP.
Here is the official federal response to SSP’s from HIV.gov.
Identification, Treatment and Prevention of Abscesses. Long but definitely worth a read (there is a summary as well). Real talk written by drug users for drug users.
Here’s an article about people who inject drugs and what the barriers are around taking PrEP.
Pre-exposure prophylaxis (PrEP) for HIV prevention among people who inject drugs: a global mapping of service delivery. We can help with PrEP referrals. If you think you’ve been exposed to HIV through sharing syringes or works, then give us a call. More info can be found on our PrEP page.
If you have suggestions for this tab that could help others, please use the form below and include a link and description and we’ll consider it.
These days, we have to assume fentanyl is in everything so it’s best to test your drugs prior to using. Here is excellent information for testing various substances (heroin, meth, MDMA). We have test strips available so please ask if you need some.
Use the right amount of citric acid to dissolve your heroin to avoid vein damage.
Opioid Overdose Basics: Recognizing and Response from The Harm Reduction Coalition. Tons of great information here.
Video of an actual overdose and someone responding with Narcan (spoiler: they save his life!). Good to watch to see how easy it is to use Narcan. Have it on hand. Overdose deaths are preventable!
Speaking of Narcan/naloxone: Naloxone (also known as Narcan®) is the drug used by paramedics to revive people who have had an opioid overdose. Naloxone can cause withdrawal symptoms and a powerful urge to take more of the drug that led to the overdose. Anyone who has been revived using naloxone should understand the risks involved in taking more drugs afterwards. Taking more drugs after being administered naloxone can result in a second overdose. This is because the half-life of naloxone (60-90 minutes) is considerably less than heroin and morphine. Drugs like methadone and sustained-release opioids such as oxycodone (brand name OxyContin) release doses of the drug slowly over 12 hours or more. So, the effect of naloxone will wear off long before those drugs have left a person’s system. More information about overdose can be found here.
If you’re interested in saving someone’s live from an opioid overdose, you can take our quick Overdose Prevention and Response training. it takes about 10 minutes and when you’re done, you’ll walk out with 2 vials of life-saving naloxone. It’s too easy not to do. Click here for more information.
“Injecting-related health harms and overuse of acidifiers among people who inject heroin…” is a study from the Harm Reduction Journal about long-term use of acidic injection solutions. It’s very in-depth and well researched.
If you have suggestions for this tab that could help others, please use the form below and include a link and description and we’ll consider it.
“This resource provides an overview of stimulants and aims to educate individuals and organizations that provide services to people who use methamphetamine and other stimulants.”
Here’s a short video with some facts about methamphetamine and amphetamines.
Meth and sexual activity can be fun and here are some tips to stay safe.
One of the OG’s when it comes to talking openly about meth use. Loads of high quality information to help you make informed decisions about meth. Tweaker.org
DanceSafe has some great info on all sorts of drugs. Check them out here.
If your veins need a break, you might try “booty-bumping“.
If you’re looking to curb your meth use, mirtazapine may help.
Syringe Services Program FAQ
Persons who inject drugs can substantially reduce their risk of getting and transmitting HIV, viral hepatitis and other blood borne infections by using a sterile needle and syringe for every injection.
Is your program anonymous?
Yes! The syringe services program is anonymous. We don’t require your name, address, phone or any other identifying information. We establish a Client ID during your first visit that will keep your identity safe.
How do I use the service?
If you are a first time user of the syringe program, we will establish your client ID. Your client ID is what we use to keep your identity anonymous at future visits.
Once established, you can come in to the syringe program and dispose of any used syringes you may have and pick up new syringes and supplies.
What if I can't bring back used syringes?
If you’re unable to bring back used syringes to our office, then dispose your syringes in our 24-hour disposal box located behind Burns St. Bistro at 1500 Burns St. If that is not an option, the next best thing is to follow these guidelines.
What else do you offer?
Lots!
- You can get tested for HIV and Hep C for FREE.
- FREE Overdose Prevention and Response Training & FREE naloxone.
- FREE Wi-Fi and power to recharge your devices.
- Housing for people living with HIV
- A clothing closet
- A safe space for everyone
What are Syringe Services Programs (SSP)?
SSPs, which have also been referred to as syringe exchange programs (SEPs), needle exchange programs (NEPs) and needle-syringe programs (NSPs) are community-based programs that provide, access to sterile needles and syringes free of cost, facilitate safe disposal of used needles and syringes, and offer safer injection education. Many SSPs also provide linkages to critical services and programs, including substance use disorder treatment programs; overdose prevention education; screening, care, and treatment for HIV and viral hepatitis; HIV pre- and post-exposure prophylaxis (PrEP); prevention of mother-to-child transmission; hepatitis A and hepatitis B vaccination; screening for other sexually transmitted diseases and tuberculosis; partner services; and other medical, social, and mental health services.
What are the benefits?
Based on existing evidence, the U.S. Surgeon General has determined that SSPs, when part of a comprehensive prevention strategy, can play a critical role in preventing HIV among persons who inject drugs (PWID); can facilitate entry into drug treatment and medical services; and do not increase the unsafe illegal injection of drugs. These programs have also been associated with reduced risk for infection with hepatitis C virus (HCV).
Many SSPs offer other infection prevention materials (e.g., alcohol swabs, vials of sterile water), condoms, and services, such as education on safer injection practices and wound care; overdose prevention; referral to substance use disorder treatment programs including medication-assisted treatment; and counseling and testing for HIV and viral hepatitis. SSPs also provide linkages to other critical services and programs, including screening, care, and treatment for HIV and viral hepatitis, HIV pre- and post-exposure prophylaxis (PrEP), prevention of mother-to-child transmission, hepatitis A and hepatitis B vaccination, screening for other sexually transmitted diseases and tuberculosis, partner services, and other medical, social, and mental health services. SSPs also protect the public and first responders by providing safe needle disposal and by reducing the number of people living with HIV and HCV infections who could transmit those infections to others.
Does having a SSP increase drug use in a community?
No. Based on existing evidence, the U.S. Surgeon General has determined that SSPs, when part of a comprehensive HIV prevention strategy, do not increase the illegal use of drugs by injection. The opportunity to expand HIV and viral hepatitis prevention services through SSPs will support communities in their efforts to identify and prevent new infections. SSPs are an effective public health intervention that can reduce the transmission of HIV and facilitate entry into drug treatment and medical services, without increasing illegal injection of drugs. SSPs often provide other services important to improving the health of persons who inject drugs (PWID), including referrals to substance use disorder and mental health services, physical health care, social services, overdose prevention and recovery support services. Studies also show that SSPs protect the public and first responders by providing safe needle disposal.